
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Mitochondrial Stress and Mitokines: Therapeutic Perspectives for the Treatment of Metabolic Diseases
- Benyuan Zhang, Joon Young Chang, Min Hee Lee, Sang-Hyeon Ju, Hyon-Seung Yi, Minho Shong
- Diabetes Metab J. 2024;48(1):1-18. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0115

- 2,051 View
- 256 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Mitochondrial stress and the dysregulated mitochondrial unfolded protein response (UPRmt) are linked to various diseases, including metabolic disorders, neurodegenerative diseases, and cancer. Mitokines, signaling molecules released by mitochondrial stress response and UPRmt, are crucial mediators of inter-organ communication and influence systemic metabolic and physiological processes. In this review, we provide a comprehensive overview of mitokines, including their regulation by exercise and lifestyle interventions and their implications for various diseases. The endocrine actions of mitokines related to mitochondrial stress and adaptations are highlighted, specifically the broad functions of fibroblast growth factor 21 and growth differentiation factor 15, as well as their specific actions in regulating inter-tissue communication and metabolic homeostasis. Finally, we discuss the potential of physiological and genetic interventions to reduce the hazards associated with dysregulated mitokine signaling and preserve an equilibrium in mitochondrial stress-induced responses. This review provides valuable insights into the mechanisms underlying mitochondrial regulation of health and disease by exploring mitokine interactions and their regulation, which will facilitate the development of targeted therapies and personalized interventions to improve health outcomes and quality of life.
- Drug/Regimen
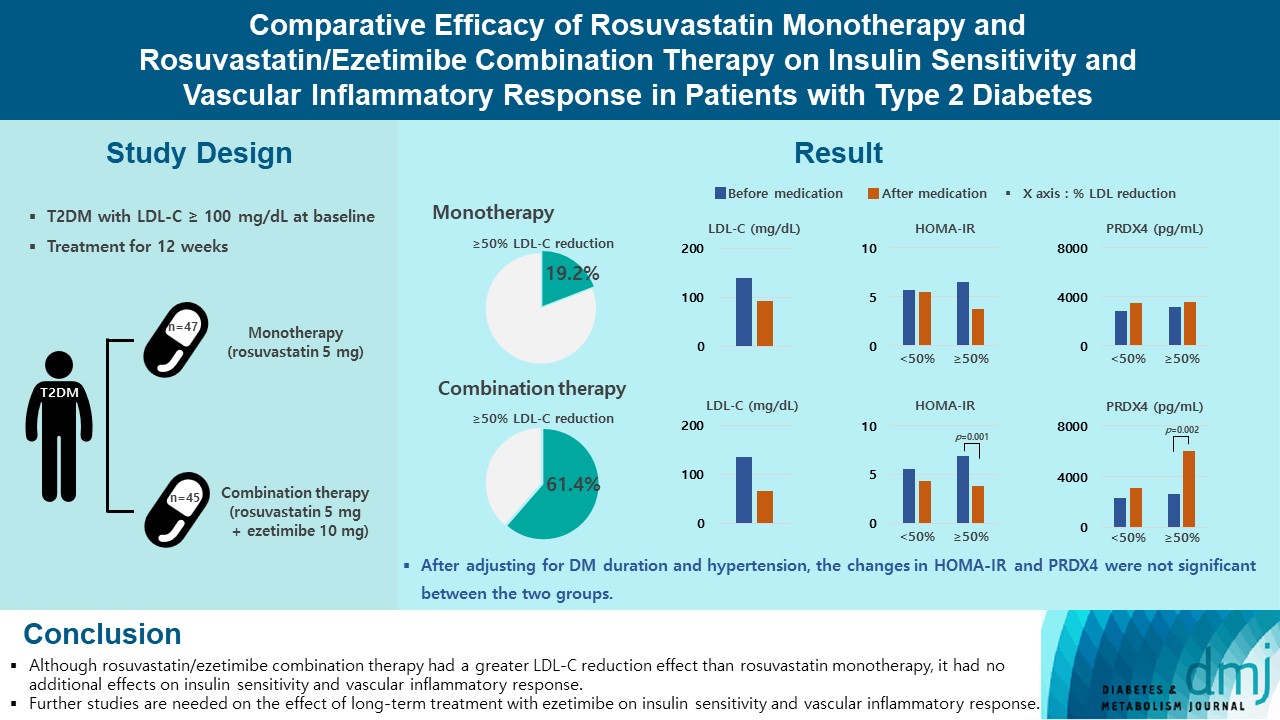
- Comparative Efficacy of Rosuvastatin Monotherapy and Rosuvastatin/Ezetimibe Combination Therapy on Insulin Sensitivity and Vascular Inflammatory Response in Patients with Type 2 Diabetes Mellitus
- Ji Hye Han, Kyong Hye Joung, Jun Choul Lee, Ok Soon Kim, Sorim Choung, Ji Min Kim, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Bon Jeong Ku, Hyun Jin Kim
- Diabetes Metab J. 2024;48(1):112-121. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0402
- 2,036 View
- 223 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes mellitus (T2DM) induces endothelial dysfunction and inflammation, which are the main factors for atherosclerosis and cardiovascular disease. The present study aimed to compare the effects of rosuvastatin monotherapy and rosuvastatin/ezetimibe combination therapy on lipid profile, insulin sensitivity, and vascular inflammatory response in patients with T2DM.
Methods
A total of 101 patients with T2DM and dyslipidemia were randomized to either rosuvastatin monotherapy (5 mg/day, n=47) or rosuvastatin/ezetimibe combination therapy (5 mg/10 mg/day, n=45) and treated for 12 weeks. Serum lipids, glucose, insulin, soluble intercellular adhesion molecule-1 (sICAM-1), and peroxiredoxin 4 (PRDX4) levels were determined before and after 12 weeks of treatment.
Results
The reduction in low density lipoprotein cholesterol (LDL-C) by more than 50% from baseline after treatment was more in the combination therapy group. The serum sICAM-1 levels increased significantly in both groups, but there was no difference between the two groups. The significant changes in homeostasis model assessment of insulin resistance (HOMA-IR) and PRDX4 were confirmed only in the subgroup in which LDL-C was reduced by 50% or more in the combination therapy group. However, after adjusting for diabetes mellitus duration and hypertension, the changes in HOMA-IR and PRDX4 were not significant between the two groups.
Conclusion
Although rosuvastatin/ezetimibe combination therapy had a greater LDL-C reduction effect than rosuvastatin monotherapy, it had no additional effects on insulin sensitivity and vascular inflammatory response. Further studies are needed on the effect of long-term treatment with ezetimibe on insulin sensitivity and vascular inflammatory response. -
Citations
Citations to this article as recorded by- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
Eun Roh
Diabetes & Metabolism Journal.2024; 48(1): 55. CrossRef
- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
- Implication of Sex Differences in Visceral Fat for the Assessment of Incidence Risk of Type 2 Diabetes Mellitus
- Sang Hyeon Ju, Hyon-Seung Yi
- Diabetes Metab J. 2022;46(3):414-416. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0089
- 2,752 View
- 154 Download
- 3 Web of Science
- 3 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Prediction of high visceral adipose tissue for sex‐specific community residents in Taiwan
Yu‐Hsuan Chang, Chin‐Sung Chang, Chieh‐Yu Liu, Yin‐Fan Chang, Shiow‐Ching Shun
Nursing & Health Sciences.2024;[Epub] CrossRef - Visceral fat and attribute-based medicine in chronic kidney disease
Hiroshi Kataoka, Kosaku Nitta, Junichi Hoshino
Frontiers in Endocrinology.2023;[Epub] CrossRef - The predictive significance of lipid accumulation products for future diabetes in a non-diabetic population from a gender perspective: an analysis using time-dependent receiver operating characteristics
Jiajun Qiu, Maobin Kuang, Yang Zou, Ruijuan Yang, Qing Shangguan, Dingyang Liu, Guotai Sheng, Wei Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Prediction of high visceral adipose tissue for sex‐specific community residents in Taiwan
- The Role of Carnitine Orotate Complex in Fatty Liver
- Hyon-Seung Yi
- Diabetes Metab J. 2021;45(6):866-867. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0272
- 4,417 View
- 110 Download
- Others
- Serum R-Spondin 1 Is a New Surrogate Marker for Obesity and Insulin Resistance
- Yea Eun Kang, Ji Min Kim, Hyon-Seung Yi, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
- Diabetes Metab J. 2019;43(3):368-376. Published online October 23, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0066
- 5,009 View
- 75 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent
in vivo studies indicated that R-spondin 1 (RSPO1) regulates food intake and increases insulin secretion, but its role in humans remains unknown. This study investigated the association between serum levels of RSPO1 and diverse metabolic parameters in humans.Methods The study population consisted of 43 subjects with newly diagnosed diabetes mellitus, and 79 non-diabetic participants. Serum levels of RSPO1 were measured using the enzyme-linked immunosorbent assay. The relationships between circulating RSPO1 and diverse metabolic parameters were analyzed.
Results Circulating RSPO1 levels increased to a greater extent in the obese group than in the lean group. Moreover, serum levels of RSPO1 were higher in the insulin-resistant group than in the insulin-sensitive group. Serum levels of RSPO1 were significantly correlated with a range of metabolic parameters including body mass index, fasting C-peptide, homeostasis model assessment of insulin resistance index, and lipid profile. Moreover, levels were significantly associated with insulin resistance and obesity in non-diabetic subjects.
Conclusion This study demonstrated the association between serum levels of RSPO1 and a range of metabolic parameters in humans. Serum levels of RSPO1 are significantly related to obesity and insulin resistance, although the precise mechanisms remain unknown.
-
Citations
Citations to this article as recorded by- LGR4: A New Receptor Member in Endocrine and Metabolic Diseases
Ningning Zhang, Mingyang Yuan, Jiqiu Wang
Endocrine Reviews.2023; 44(4): 647. CrossRef - R-Spondin1 and tumor necrosis factor-alpha in infertile women with polycystic ovary syndrome: relationships with insulin resistance and other parameters
Tuğba GÜRBÜZ, Oya GÖKMEN, Asena AYAR MADENLİ, Berna DİLBAZ
Journal of Health Sciences and Medicine.2023; 6(2): 449. CrossRef - An early prediction model for type 2 diabetes mellitus based on genetic variants and nongenetic risk factors in a Han Chinese cohort
Jinjin Li, Qun Ye, Hongxiao Jiao, Wanyao Wang, Kai Zhang, Chen Chen, Yuan Zhang, Shuzhi Feng, Ximo Wang, Yubao Chen, Huailin Gao, Fengjiang Wei, Wei-Dong Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Emerging Therapeutic Strategies for Attenuating Tubular EMT and Kidney Fibrosis by Targeting Wnt/β-Catenin Signaling
Lichao Hu, Mengyuan Ding, Weichun He
Frontiers in Pharmacology.2022;[Epub] CrossRef - Does Serum R-Spondin-1 Play a Role in PCOS Pathophysiology?
Osman BAŞPINAR, Yasin ŞİMŞEK, Derya KOÇER, Oğuzhan Sıtkı DİZDAR, Hatice KAYIŞ TOPALOĞLU
Genel Tıp Dergisi.2022; 32(5): 490. CrossRef - Silencing of RSPO1 mitigates obesity-related renal fibrosis in mice by deactivating Wnt/β-catenin pathway
Xuesong Su, Guangyu Zhou, Mi Tian, Si Wu, Yanqiu Wang
Experimental Cell Research.2021; 405(2): 112713. CrossRef - Exosome miR‐27a‐3p secreted from adipocytes targets ICOS to promote antitumor immunity in lung adenocarcinoma
Xuehan Fan, Jingya Wang, Tingting Qin, Yujia Zhang, Wenting Liu, Kaiting Jiang, Dingzhi Huang
Thoracic Cancer.2020; 11(6): 1453. CrossRef - Integrative Analyses of Genes Associated with Subcutaneous Insulin Resistance
Manoj Kumar Pujar, Basavaraj Vastrad, Chanabasayya Vastrad
Biomolecules.2019; 9(2): 37. CrossRef
- LGR4: A New Receptor Member in Endocrine and Metabolic Diseases
- Others
- Effect of Atorvastatin on Growth Differentiation Factor-15 in Patients with Type 2 Diabetes Mellitus and Dyslipidemia
- Ji Min Kim, Min Kyung Back, Hyon-Seung Yi, Kyong Hye Joung, Hyun Jin Kim, Bon Jeong Ku
- Diabetes Metab J. 2016;40(1):70-78. Published online February 19, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.1.70
- 4,173 View
- 33 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Elevated serum levels of growth differentiation factor-15 (GDF-15) are associated with type 2 diabetes. Therefore, the effects of atorvastatin on metabolic parameters and GDF-15 levels in patients with type 2 diabetes and dyslipidemia were evaluated.
Methods In this prospective randomized trial from February 2013 to March 2014, 50 consecutive type 2 diabetic patients with a low density lipoprotein cholesterol (LDL-C) levels ≥100 mg/dL were enrolled. The patients were divided into two groups based on the amount of atorvastatin prescribed, 10 mg/day (
n =23) or 40 mg/day (n =27). The effect of atorvastatin on metabolic parameters, including lipid profiles and GDF-15 levels, at baseline and after 8 weeks of treatment were compared.Results The baseline metabolic parameters and GDF-15 levels were not significantly different between the two groups. After 8 weeks of treatment, the total cholesterol (TC) and LDL-C levels were significantly decreased in both groups. The mean changes in TC and LDL-C levels were more significant in the 40 mg atorvastatin group. The GDF-15 level was decreased in the 10 mg atorvastatin group, from 1,460.6±874.8 to 1,451.0±770.8 pg/mL, and was increased in the 40 mg atorvastatin group, from 1,271.6±801.0 to 1,341.4±855.2 pg/mL. However, the change in the GDF-15 level was not statistically significant in the 10 or 40 mg atorvastatin group (
P =0.665 andP =0.745, respectively).Conclusion The GDF-15 levels were not significantly changed after an 8-week treatment with atorvastatin in type 2 diabetic patients.
-
Citations
Citations to this article as recorded by- The relationship of Growth differentiation factor-15 with renal damage and dyslipidemia in non-albuminuric and albuminuric Type-2 Diabetes Mellitus
Hasan Esat Yücel, Bilal İlanbey
Medical Science and Discovery.2022; 9(6): 334. CrossRef - Comparative effectiveness of statins on non-high density lipoprotein cholesterol in people with diabetes and at risk of cardiovascular disease: systematic review and network meta-analysis
Alexander Hodkinson, Dialechti Tsimpida, Evangelos Kontopantelis, Martin K Rutter, Mamas A Mamas, Maria Panagioti
BMJ.2022; : e067731. CrossRef - The Cytokine Growth Differentiation Factor-15 and Skeletal Muscle Health: Portrait of an Emerging Widely Applicable Disease Biomarker
Boel De Paepe
International Journal of Molecular Sciences.2022; 23(21): 13180. CrossRef - Biomarkers of subclinical atherosclerosis in patients with psoriasis
Hannah Kaiser, Xing Wang, Amanda Kvist-Hansen, Martin Krakauer, Peter Michael Gørtz, Benjamin D. McCauley, Lone Skov, Christine Becker, Peter Riis Hansen
Scientific Reports.2021;[Epub] CrossRef - Growth differentiation factor-15 regulates oxLDL-induced lipid homeostasis and autophagy in human macrophages
Kathrin Ackermann, Gabriel A. Bonaterra, Ralf Kinscherf, Anja Schwarz
Atherosclerosis.2019; 281: 128. CrossRef
- The relationship of Growth differentiation factor-15 with renal damage and dyslipidemia in non-albuminuric and albuminuric Type-2 Diabetes Mellitus

 KDA
KDA
 First
First Prev
Prev





